Unlocking Equity: Transforming Rural California's Organ Transplant System
- Gayathri Mungi

- Oct 19, 2023
- 11 min read
In our exploration of the intricate dynamics of the organ transplant system and its impact on predominantly rural areas, we are privileged to introduce Gayathri Mungi – a tireless advocate for sustainable development within her community. Her commitment to empowering others and fostering positive change embodies the essence of our quest.
Gayathri, a Troy Tech and IB first decile student at one of the United States' premier public high schools, is not merely an academic achiever; she is a catalyst for change. With prestigious accolades from institutions like Columbia University and the Johns Hopkins Center for Talented Youth, she passionately engages in geospatial research. Currently, she's illuminating the organ transplant disparities among rural California residents through an insightful story map created with ArcGIS. Her work not only enhances our collective understanding but also aligns seamlessly with the Sustainable Development Goals (SDGs), setting a new standard for community-driven research and advocacy.
The current organ transplant system inefficiency, illuminated by research publications in early 2023, disproportionately affects rural Americans. They are up to 20% less likely to receive essential transplants, a stark contradiction to SDG 3 (Good Health and Well-being) and SDG 10 (Reduced Inequalities).
Our research uncovers four essential strategies to address these barriers and advance SDGs: prevention and community engagement (SDG 3), improving access to nutritious food (SDG 2), expanding medical and educational infrastructure (SDG 4 and SDG 10), and addressing physician shortages (SDG 3 and SDG 17).

The collective effort towards these strategies ensures a healthier and more equitable future for all Californians, echoing the principles of the SDGs.
In early 2023, a new cycle of articles from sources like UPenn to Bloom Works published on the inefficiency of the current organ transplant system. According to a UPenn research update, up to 28,000 potentially lifesaving organs are not recovered from deceased donors while over 6,000 patients a year do not receive life-saving organs due to the inefficiency of the current system (Tachibana, 2023). Making matters worse, rural Americans face a disproportionate number of hurdles in accessing organs in an inefficient and inequitable system; they are up to 20% less likely to receive heart, kidney, or liver transplants in comparison to urban residents (Conlon 2008).
According to CDC research, residents of predominantly rural counties (counties in which greater than 50% of the population is a rural resident) in California are poorer, unhealthier, and more isolated than ever before. Rural residents are more likely to die from cardiovascular disease, cancer, and stroke than their urban counterparts (CDC, 2023). There are over 1.8 million people in California that are considered rural residents. The problems that rural Californians face start long before requiring an organ transplant. It starts with health-related behaviors, their environment, and systemic inequalities (CDC, 2013).
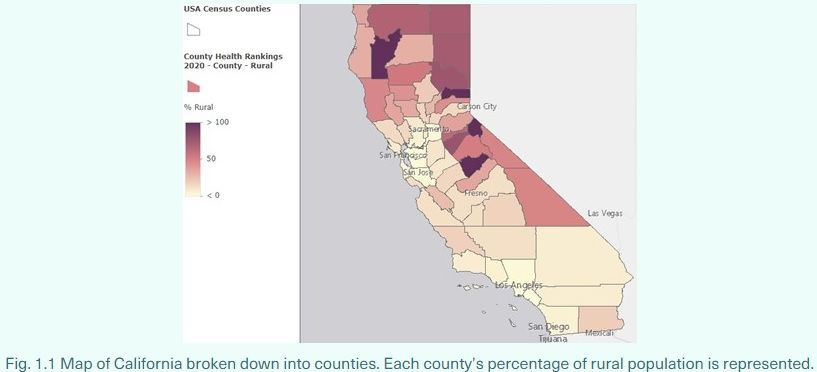
The focus of this research will be on predominantly rural counties in California. Those counties are Siskiyou County, Tehama County, Amador County, Modoc County, Lassen County, Plumas County, Calaveras County, Sierra County, Trinity County, Mariposa County and Alpine County.

Health-Related Behaviors
Tobacco Use
The effects of tobacco consumption and second-hand smoke cause significant cardiovascular damage, resulting in the need for lung and/or heart transplants. Approximately 7.2% of adult residents of predominantly rural counties are considered current smokers (adults who smoke most to all days), 0.6% lower than the state average (University of Wisconsin Population Health Institute, Robert Wood Johnson Foundation, 2022).
Obesity
Over 26% of the adult population in these predominantly rural counties are obese, compared to the 21% state average adult obesity rate (University of Wisconsin Population Health Institute, Robert Wood Johnson Foundation, 2022). Obesity can cause a plethora of health problems or exacerbate existing problems. Furthermore, obesity can become an epigenetic condition, which can harm future generations.
In addition, a study by Project Implicit 2013 found that 40% of medical students have unconscious bias against obese people, a bias that is likely to continue to develop throughout the physician’s career, which can prevent obese patients from receiving proper care (Stanford School of Medicine | Unconscious Bias in Medicine, 2017).
Environment Factors
Air Pollution
A recent study also found that air pollution particles are more dangerous in rural areas than in urban areas as they measured the toxicity of the particle, not just the count of particles in the air. This study found that there were spikes in these toxins during peak agriculture seasons. As rural Californians produce necessities for millions of Americans, they are releasing billions of toxins that have the potential to cause significant lung damage (Cronin, 2022).
Although residents of predominantly rural counties smoke less, they have higher rates of chronic lower respiratory disease and cardiovascular damage, possibly caused by the worse toxicity of air pollution (CDC, 2023).
Systemic Inequalities
Food Insecurity
Despite rural California being responsible for producing most of the US’s agriculture commodities, many of these predominantly rural counties have limited access to fresh fruits and vegetables (Breadbasket Of The World, 2023). Nutritious food is vital to living a healthy lifestyle and mitigating health problems.
California’s food stamps program, CalFresh, aims to provide benefits to low-income households, acting as a safety net for them (CDSS Programs | CalFresh, 2023). However recent research from Health & Place found that CalFresh lacks substantial infrastructure in rural California. Significant portions of rural California lack bandwidth infrastructure making it difficult for rural residents to access online benefits and physical infrastructure (i.e., roads) making food delivery difficult. CalFresh coverage is significantly greater in urban areas than in rural areas, contributing to health factor disparities (Foster et al., 2022). This reflects broader trends of rural Americans facing greater difficulties in accessing beneficial health factors which can contribute to worse health outcomes.


Poverty
The poverty rate in predominantly rural counties, on average, is higher than the state poverty rate (University of Wisconsin Population Health Institute, Robert Wood Johnson Foundation, 2022). This means that rural residents are less likely to have health insurance and financial stability, making it more difficult for them to access health care. Studies have also found that poverty contributes to medical bias that prevents impoverished patients from receiving the full breadth of necessary care (Stanford School of Medicine | Unconscious Bias in Medicine, 2017). In the case of the organ transplant system, impoverished patients are considered to be more high-risk as it less likely they are able to afford the support system and routine necessary to ensure success after the transplant. As a result, they are less likely to get a transplant because it is deemed to be more likely a failure.

There are numerous disparities amongst the impoverished. Racial minorities are much more likely to experience poverty than their white counterparts (University of Wisconsin Population Health Institute, Robert Wood Johnson Foundation, 2022). Children in poverty are likely part of households in poverty which brings forth the concern of multi-generational effects of poverty. These household poverty rates can be extrapolated to be indicative of poverty rates amongst different racial/ethnic groups, despite age. These differences can further exacerbate disparities in access to healthcare and treatment.

Inaccessibility and Inefficiency
As mentioned before there exist a significant number of barriers and factors that harm rural residents. Adding to these barriers is the inaccessibility of active transplant centers to these rural residents. Active transplant centers are in only a few counties in California: San Francisco, Orange, Los Angeles, Santa Clara, Sacramento, San Diego, Riverside, and San Bernardino County (OPTN, 2023). It is incredibly difficult for people that live in Central California or in the most northern counties of California. There is the physical distance but there is also financial insecurity and/or lack of insurance that prevent residents from receiving care (Conlon, 2008).

Fig. 4.1 This map shows all the active transplant centers in California. They are located in metropolitan areas. It is incredibly difficult to access these centers due to physical distance, lack of infrastructure, poverty, and/or lack of insurance.
There is a physician shortage in rural California, making it difficult for potential patients to meet with primary care physicians. Limited physical infrastructure, medical personnel, and clinics/hospitals make it difficult for rural residents to access resources on healthy behaviors and treatment. (CDC, 2013). HRSA considers residents of rural areas as “geographically isolated and economically or medically vulnerable”, resulting in poorer health outcomes. (HRSA, 2020).
Deadly medical bias based on systemic racism and sexism, as well as bias against the impoverished, can prevent a medical professional from adequately caring for a patient (Stanford School of Medicine | Unconscious Bias in Medicine, 2017). For example, the California Health Care Foundation found that almost a third of Black Californians report being treated unfairly due to race, ethnicity, mental health, sexuality, disability, and/or gender (Cummings, 2022). In relation to the organ transplant system, implicit biases have been shown to delay specialist referrals, evaluations (a patient can only be added to the organ waiting list if they are evaluated by a specialist and deemed a fit candidate for the process), and transplants which can lead to deadly outcomes (Hackmann, 2022).
Findings & Conclusion
Health Factors and Health Outcomes
Health factors have a strong correlation with health outcomes. The identified predominantly rural counties have below average state rankings of health factors and outcomes of 43.09 and 43.18, respectively. The average state ranking for both is 29.5 (University of Wisconsin Population Health Institute, Robert Wood Johnson Foundation, 2022). What is even more concerning is that the state rankings of health factors appear to have little correlation with the state ranking of health outcomes, indicating that there are external factors (clinical care, social & economic environment, and physical environment) that are significantly contributing to these worse than average health outcomes. To make the healthcare system, with a focus on the organ transplant system, more equitable it is important to address risk factors, lower socioeconomic status, poor insurance coverage, and lack of quality healthcare.
Solutions
This study has identified four main ways to address these barriers that rural communities face in accessing quality health care and transplant services.
The most impactful way to improve the health outcomes of rural residents lies in prevention. This means engaging rural residents in health initiatives to improve their health and lifestyle behaviors, including educating rural residents about the dangers of smoking, alcohol abuse, obesity and other risky behaviors. More than just educating stakeholders, it is important to create a community of health minded individuals. In the African American community, California Health Equity Initiatives have successfully set up Health Ministries with Nurse Corps to create a community of informed and engaged individuals. Improving one’s health isn’t just an individual task but requires the support of a community. Culturally informed initiatives allow people to be regularly engaged and would support positive changes in lifestyle like engaging in a balanced diet, physical activity, and caring for mental/emotional wellbeing (Hackmann, 2022). These communities could act as the first line of defense and can save lives.
One way to improve health-related behaviors is to make nutritious food more accessible through programs like CalFresh. Through the creation of community hubs for food to be dropped off and be bought by rural residents and decreasing the digital divide that harms rural Californians (Foster et al., 2022). Another way to make nutritious food more accessible is through local initiatives like farmer’s markets and food banks. An additional local option is the implementation of library garden programs. Utilizing state funding and resources, libraries can provide the supplies, tools, and education to their community members to empower them to contribute to the community garden or private garden that provides fresh and nutritious produce (Web Junction | Growing Library Garden Programs, 2023). Up taking these preventative measures does not mean that organ transplant services are not necessary, but there are ways for rural residents to improve their overall health to prevent or delay the severity of disease that would require such services.
Another important step is developing the medical centers of the University of California (UC) and California State University (CSU) systems further. For the UC system specifically, it is important to develop UC Merced similar to the other UC’s medical centers. Many transplant centers in California are based out of the UCs. Opening a transplant center or a medical center through UC Merced or additional satellite centers in rural California would provide lifesaving treatments for thousands of people. It is important to expand the CSU system either by building more colleges into the system or expanding the reach of the existing schools with more satellites. Making higher education more accessible, especially for potential students that live in rural California, would decrease poverty and increase informed behaviors in newer generations. The educated will be able to implement positive change in their communities, potentially improving health factors and outcomes. In addition, many CSU campuses have health clinics that are free to students that pay a fee and accept Medi-Cal and Covered California (Cal State Student Health Services, 2023). This would make healthcare much more accessible to rural residents as they could access clinics for a reduced cost. Even if the clinic is not of the same scale as other hospitals and clinics it would be able to address the needs of nearby residents.

Finally, it is important to address the physician shortage in rural areas. All the predominantly rural counties are assigned medium priority for assignment of clinicians. By increasing the number of accessible physicians in a predominantly rural area, 2,000 people per added full-time equivalent (FTE) physician would directly benefit. Traveling physicians and telehealth options would be a good way to introduce more full-time equivalent physicians to areas in need. Below are predominantly rural counties listed with the number of FTE physicians (and associated personnel, clinics, and supplies) needed to serve the area to pull them out of a danger zone (HRSA, 2023). By making physicians and healthcare more accessible to these rural counties it would greatly improve health outcomes and make the healthcare system more equitable.
§ Siskiyou County – 5
§ Tehama County – 9
§ Amador County - 3
§ Modoc County - 2
§ Lassen County – 2
§ Plumas County – 3
§ Calaveras County - 1
§ Sierra County - 1
§ Trinity County - 2
§ Mariposa County – 4
§ Alpine County - 1

Future Research
To build on the HRSA recommendations, it is important to locate high population density areas and place permanent clinics there as needed. Policymakers should consider the development of telehealth and traveling clinic options in rural areas in order to effectively and efficiently serve those in need.
Bibliography
“About Rural Health.” Centers for Disease Control and Prevention, 9 May 2023, www.cdc.gov/ruralhealth/about.html.
Axelrod, David A, et al. “Rates of Solid-Organ Wait-Listing, Transplantation, and Survival Among Residents of Rural and Urban Areas.” JAMA Network, 9 Jan. 2008, Accessed 7 June 2023.
Bazargan, Mohsen et al. “Discrimination and Medical Mistrust in a Racially and Ethnically Diverse Sample of California Adults.” Annals of family medicine vol. 19,1 (2021): 4-15. doi:10.1370/afm.2632
“Breadbasket Of The World.” EB5 Northern California - Breadbasket of the World, eb5northerncalifornia.com/index.php?page=breadbasket-of-the-world. Accessed 23 July 2023.
Conlon, Michael. “Rural U.S. Faces Organ Transplant Hurdles: Study.” Reuters, 8 Jan. 2008.
“CDSS Programs | CalFresh.” CDSS, www.cdss.ca.gov/inforesources/calfresh. Accessed 24 July 2023.
Cronin, Dana. “The Air in Rural Areas May Be Just as Toxic as the Pollution in Cities.” KCUR, 31 Jan. 2022, www.kcur.org/news/2022-01-31/the-air-in-rural-areas-may-be-just-as-toxic-as-the-pollution-in-cities.
Cummings, Linda. “Listening to Black Californians: How the Health Care System Undermines Their Pursuit of Good Health.” California Health Care Foundation, 4 Oct. 2022, www.chcf.org/publication/listening-black-californians-how-the-health-care-system-undermines-their-pursuit-good-health/.
Esri_Demographics. “Rural California County Data” [Light Gray Base Map]. Scale Not Given. “County Health Rankings 2020”. June 3, 2022. https://services.arcgis.com/P3ePLMYs2RVChkJx/arcgis/rest/services/CountyHealthRankings2020_WFL1/FeatureServer. (July 25, 2023).
Federal_User_Community. “Rural California County Data” [Light Gray Base Map]. Scale Not Given. “Health Professional Shortage Areas in Primary Care Designation Boundaries”. June 30, 2023. https://services2.arcgis.com/FiaPA4ga0iQKduv3/arcgis/rest/services/Health_Professional_Shortage_Areas_in_Primary_Care_Designation_Boundaries/FeatureServer . (July 25, 2023).
Foster, Isabelle S, et al. “Disparities in Snap Online Grocery Delivery and Implementation: Lessons Learned from California during the 2020-21 Covid Pandemic.” Health & Place, July 2022, www.ncbi.nlm.nih.gov/pmc/articles/PMC9122786/.
“Growing Library Garden Programs.” WebJunction, 27 June 2023, www.webjunction.org/news/webjunction/growing-library-garden-programs.html.
Hackmann, M. “Confronting and Eliminating Inequities in the Organ Transplantation System.” Realizing the Promise of Equity in the Organ Transplantation System, NATIONAL ACADEMIES PRESS, Washington D.C., 2022.
“Health-Related Behaviors by Urban-Rural County Classification - United States, 2013.” Centers for Disease Control and Prevention, 14 Mar. 2023, www.cdc.gov/mmwr/volumes/66/ss/ss6605a1.htm .
NIH/National Heart, Lung and Blood Institute. "Risk of developing heart failure much higher in rural areas vs. urban." ScienceDaily. ScienceDaily, 25 January 2023. <www.sciencedaily.com/releases/2023/01/230125121545.htm>.
“Student Health Services.” The California State University, www.calstate.edu/attend/student-services/Pages/student-health-services.aspx. Accessed 24 July 2023.
Tachibana, Chris. “Reforming Unos to Improve Organ Allocation.” Penn LDI, 30 May 2023, ldi.upenn.edu/our-work/research-updates/ending-unoss-monopoly-over-the-u-s-organ-transplant-system/.
“Transplant Centers.” Organ Procurement and Transplantation Network, optn.transplant.hrsa.gov/about/search-membership/?memberType=Transplant%2BCenters&state=-1®ion=0. Accessed 26 July 2023.
“Unconscious Bias in Medicine.” Stanford Center for Continuing Medical Education. Unconscious Bias in Medicine, 8 June 2023, Palo Alto, https://stanford.cloud-cme.com/course/courseoverview?P=0&EID=20775 . Accessed 8 June 2023.
Williams, David R, and Ronald Wyatt. “Racial Bias in Health Care and Health Challenges and Opportunities.” JAMA Network , vol. 314, no. 6, 11 Aug. 2015, pp. 535–638, https://doi.org/10.1001 .



Comments